CGM Accuracy Matters
Your Guide to Choosing a Reliable Continuous Glucose Monitor (CGM)
What are CGMs?
Continuous glucose monitors (CGMs) are wearable medical devices used by people with diabetes to monitor glucose levels in real time. The sensor sends this information wirelessly to a smartphone app, where users can see their glucose readings, track trends, and get alerts if their glucose levels go too high or too low. CGMs help people with diabetes make immediate, informed decisions about food, exercise, and medication.
How do you know which CGM to choose?
With so many new CGMs on the market, it can be hard to know which one to choose. We want you to feel informed and supported as you explore your options.
Right now, there are no global standards to ensure all continuous glucose monitors (CGMs) are tested in the same way before they reach the market. ISO standards (International Organisation for Standardisation) are used for traditional blood glucose meters, but they aren’t applied to CGMs. That means some CGM devices can be approved and sold without going through the same level of rigorous testing as others.
While many are accurate and safe, others might not have been studied as thoroughly in real-life settings or across different groups of people living with diabetes.
This is why it’s so important to look at how each CGM was tested and how well it performs day to day, not just what’s written on the packaging. Understanding this helps you make sure your CGM gives you glucose readings you can trust.
Why does CGM accuracy matter?
CGM accuracy is really important because the numbers you see from your CGM guide your daily diabetes decisions. It's important to know:
Not all CGMs are created equally
Some are more accurate than others. A good CGM gives glucose readings that are very close to your actual blood sugar levels.
The impact now
If your CGM readings are not accurate, you could miss or wrongly treat dangerous glucose events, like very high or very low glucose levels. This can lead to diabetic ketoacidosis (DKA) or severe hypoglycaemia, both serious and potentially life-threatening if not managed in time.
The impact later
Over time, inaccurate readings can lead to glucose levels being out of the recommended range (between 3.9-10.0mmol/l) too often, which increases the risk of long-term complications like eye, kidney, or nerve problems.
Let’s dive a little deeper:
Different CGM systems can show very different numbers, not because your body is different, but because some sensors read higher or lower than your true glucose levels.
During a CGM Accuracy study, some CGMs are tested against fingerstick (capillary) blood, while others are compared to blood samples that a laboratory uses (venous blood). This matters because lab blood usually shows lower glucose levels than the fingerstick blood.
How CGM testing works: A simple story
When a new CGM is tested, researchers want to see how close its readings are to your real blood glucose levels. Let’s imagine two people, Thabo and Aisha, who are part of a study that is testing a new CGM device.
Not all CGMs are created equally

Thabo’s study: compared to fingerstick blood (capillary):
Thabo wears a new CGM on his arm for several days. Throughout the day, he does lots of fingerstick tests, sometimes every 15 to 30 minutes! Each time, he notes the reading from his fingerstick test and the number showing on his CGM at that exact moment.
Researchers then compare these two readings to see how close the CGM is to real fingerstick blood sugar levels.
This type of study gives a good picture of how the CGM performs in everyday life, since it matches what people actually do at home.
Aisha’s study: compared to lab blood (venous):
Aisha’s study takes place in a hospital or research clinic. She’s also wearing a CGM, but instead of doing fingerstick tests, nurses draw blood from her arm (venous blood) at regular times, maybe every 15 to 30 minutes for several hours.
That blood is sent to a laboratory, where scientists measure glucose using very accurate equipment. These lab results are then compared to the CGM readings taken at the same time.
This gives researchers a sense of how the CGM performs against precise lab measurements, but it’s less like real life and sometimes lab blood shows lower glucose levels than fingerstick blood.
Let’s look at another example. Would you change your food, insulin or exercise regimen if your CGM showed the blue line in the picture to the right? What if it showed the red line? Would your decisions be the same?
Remember, it is the fingerstick glucose level that shows the true glucose highs your body is really exposed to. And that’s the one you use when making day-to-day decisions about food, insulin and exercise. That’s part of why some CGMs might seem more accurate in studies than they feel in real life; it depends on what kind of blood they were compared to. Knowing how a CGM was tested helps you understand what its numbers really mean for your day-to-day care.
Why this matters
Both study types are valuable, but they can give different results.
A CGM tested against lab blood might look more accurate on paper, but in real life, it could show numbers that are a bit lower than what your body actually experiences.
A CGM tested against fingerstick blood tends to reflect real-world readings more closely, because that’s what people use for daily diabetes decisions at home.
It’s going to impact you now because CGMs are a key part of daily diabetes care. They show how your food, sleep, stress, and exercise affect your glucose levels, helping you recognise patterns that help you make informed decisions about your diabetes management
If your CGM isn’t accurate, it might miss or show false glucose levels, and that can be dangerous.
If your CGM says you’re fine but your glucose is actually very high, you might not take insulin when needed. This can lead to diabetic ketoacidosis (DKA), a serious condition that can land you in the hospital.
If your CGM says you’re low when you’re not, you might eat unnecessarily or take less insulin, making it harder to stay in a safe range.
If it misses a real low, you could have severe hypoglycaemia, a medical emergency that can cause confusion, loss of consciousness, seizures, and, in extreme cases, can be life-threatening if not treated immediately.
The impact now
It’s going to impact you later because inaccurate CGM readings can keep your glucose levels out of range without you realising it, increasing the risk of future complications affecting your eyes, kidneys, nerves, and heart. This shows just how important reliable, well-tested devices are for your long-term health as a person living with diabetes.
Over time, if your CGM isn’t accurate, your glucose levels might stay outside the recommended Time In Range (3.9–10.0 mmol/L) more often than you realise.
This can increase your risk of long-term complications that affect your eyes, kidneys, nerves, and heart.
Devices that haven’t been properly tested might show glucose readings that are too high or too low, giving a false Time in Range (TIR).
Time in Range means how much of your day your glucose stays in the green zone, kind of like keeping your car’s speed within the speed limit.
Doctors recommend aiming to be in range at least 70% of the time (around 17 hours a day) to help lower your risk of long-term diabetes complications.
CGM accuracy matters for research and new treatments. These devices are used to test how well new drugs or therapies work, so all CGMs must measure glucose in the same, reliable way.
The impact later
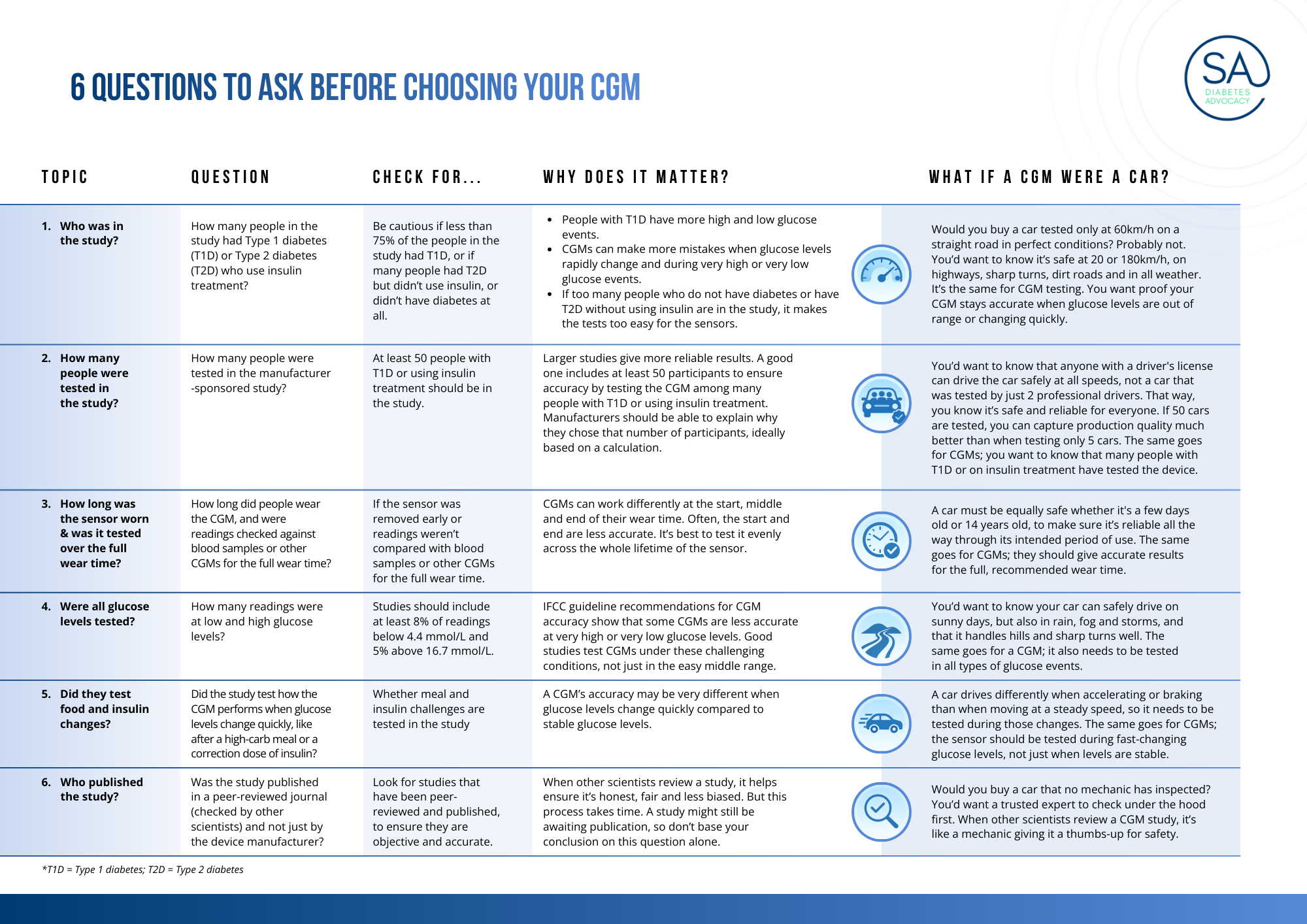
6 questions to ask before choosing your CGM
To address the above concerns, SA Diabetes Advocacy, in partnership with FIND, IfDT and SEMDSA, developed an interim guide called the CGM Performance Factsheet, consisting of 6 questions that you can ask to help you make an informed decision about which CGM on the market is best for you, by:
Asking the right questions about how the CGM was tested
Knowing if the CGM study included the right people
Understanding if you can trust the CGM’s glucose readings
Below, we have adapted the FIND Checklist and added a car analogy:
Think of your CGM like a car; you wouldn’t buy one that hadn’t been properly tested for safety and performance. The same goes for a CGM. It needs to be tested to make sure it gives accurate readings you can trust every day.
Some “cars” (or CGMs) might look great, but if they haven’t been tested in real-life conditions like traffic, rain, or different road types, you don’t really know how safe they are. Reliable CGMs are tested under real-world conditions such as different temperatures, physical activity, meals, and sleep, and across different ages and types of diabetes.
Just like safe cars, well-tested CGMs go through these challenges to prove they work accurately and reliably for everyone, every day.
How do I safely use a new CGM device?
Discuss your CGM choice with your healthcare team and follow the CGM instructions and training guides.
In the beginning, check your CGM readings against fingerstick tests or a reliable CGM device that you are confident about, especially if something feels off or your symptoms don’t match your readings.
Always have a backup glucose meter ready in case your CGM stops working or gives unexpected readings.
How to report a faulty CGM device?
If you encounter a faulty sensor for your CGM device in South Africa, here’s how to report it:
Remove the sensor and keep all packaging, serial numbers, and usage log/screenshots to support your report.
Contact the distributor or manufacturer of the device: explain the fault, provide the device number, and ask for their instructions on returning the device or getting a replacement. The distributor's information should be available online or on the CGM website.
If the fault could be considered an adverse event (for example, the sensor gave dangerously inaccurate readings, caused harm or had major performance issues), you or your healthcare provider can report it to the South African Health Products Regulatory Authority (SAHPRA).https://www.sahpra.org.za/health-products-vigilance/
Email: mdvigilance@sahpra.org.za
Telephone: 012 501 0476You may need to fill in the “Medical Device Adverse Event Reporting Form (GLF-MD-11A)” and follow the guidelines.
When reporting, include as much detail as you can: device name, model, lot/serial number, what went wrong, when and how it happened, and your contact information.
Keep records of your communication with the manufacturer/distributor and SAHPRA, as it can be important for follow-up or recall actions.
References and special thanks
It takes a village to simplify these messages for the diabetes community. Thank you to everyone who took the time to review this work and help us understand CGM accuracy better so that we can help empower PLWD through education.
John Pemberton, Glucose never lies
Cathy Haldane, FIND
Stefan Pleus, IfDT, Germany for the car analogy
Priyanka Singh, FIND
SEMDSA
Diabetes Alliance
Sweet Life
Link to FIND CGM Performance Factsheet: https://www.finddx.org/wp-content/uploads/2026/02/20260202_FIND_CGM-FACTSHEET_V2.pdf
Link to CGM Systems for Insulin Dosing Comparison Chart: https://static1.squarespace.com/static/636e507501d1fa72da31dd2d/t/68dcec7d31babe57cad64f55/1759308925834/DSN+CGM+Comparsion+Charts+-+1.10.25.pdf
As mentioned in: https://www.dailymaverick.co.za/article/2025-10-01-the-imperative-for-medical-device-regulation-to-ensure-safety-and-efficacy-in-healthcare/